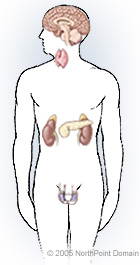
Incontinence, the involuntary loss of urine, is a symptom of an underlying problem and not a medical condition itself. Once the underlying problem has been addressed, incontinence will stop. Underlying conditions that cause incontinence include:
- Infection;
- Inflammation;
- Urinary obstruction;
- Muscle weakness;
- Nerve damage;
- Anatomical abnormality; and
- Physical or mental disability.
The first step in treating incontinence is to define the type of incontinence, such as:
- Stress incontinence;
- Urge incontinence;
- Reflex incontinence;
- Overflow incontinence; or
- Functional incontinence.
PRE-TREATMENT GUIDELINES
A bladder diary can help the physician identify the type of incontinence. After reviewing a bladder diary, the physician reviews the results of any urinary diagnostic tests, including:
- Urodynamics testing;
- Post-void residual volume; and
- Ultrasound.
WHAT TO EXPECT
Treatment often begins with behavioral modification. If this approach fails, the physician may recommend medication or surgery.
Timed voiding. To control urge incontinence, physicians may first recommend urinating according to a regular schedule.
Kegel exercises. Kegel exercises are voluntary contractions that strengthen the pelvic floor muscles.
Vaginal cones. Weighted vaginal cones are another method of improving pelvic muscle tone. The patient holds these cones in the vagina for as long as possible.
Biofeedback. A biofeedback apparatus can stimulate the pelvic floor muscles to help a patient locate them. Biofeedback may be done in conjunction with Kegel exercises.
Electrical stimulation. Electrical stimulation involves attaching electrical probes to the pelvic floor muscles and sends a light electrical shock to the muscles, forcing them to contract.
NeoControl chair. The NeoControl Chair uses electromagnetic waves that are pulsed through the skin to stimulate the pelvic muscles to contract.
Devices
Patients may need to wear a pad or device to curb or absorb urine leakage, including:
- Pessary;
- Miniature patch;
- Urethral plug; and
- Catheter.
Medications
Common medications to treat urinary incontinence include:
- Alpha-adrenergic agonists;
- Calcium channel blockers;
- Anticholinergics; and
- Alpha-adrenergic antagonists.
Surgery
Surgical interventions include:
Burch/Marshall-Marchetti-Kranz (Burch/MMK) retropubic suspension. In this procedure, the physician sews the vaginal wall or bladder (sometimes both) to the pelvic bone to support the urethra.
Sling procedure. A surgeon constructs a hammock of synthetic material or body tissue to support the bladder neck.
Bulking agent. Physicians sometimes inject a bulking agent, such as bovine collagen (Contigen) or Durasphere, into the urethral sphincter.
Implantable devices. Implantable nerve stimulation devices are anchored in the abdominal wall and send small electrical impulses to the sacral nerves to help control bladder contractions.
POSSIBLE COMPLICATIONS
Devices
The possible complications from devices include:
- Vaginal discharge;
- Pain on insertion and removal;
- Tears in the vaginal lining;
- Painful intercourse;
- Infection;
- Urethral opening stretching;
- Urethral sphincter damage;
- Bladder stones;
- Bladder infection; and
- Urethral erosion.
LIFESTYLE ADJUSTMENTS
Lifestyle changes that a physician may recommend include:
- Avoiding foods that can cause incontinence symptoms;
- Limiting alcohol and caffeine consumption;
- Spacing drinks throughout the day;
- Maintaining an appropriate weight;
- Taking vitamins and promoting general good health;
- Exercising regularly; and
- Quitting smoking.