Urodynamics
Basic Facts
-
- Urodynamics, also known as bladder function studies, is a series of tests that assess the neuromuscular responses of the bladder to filling and emptying.
-
- Urodynamic probes insert into the urethra, bladder, rectum, or vagina, causing little discomfort.
-
- Combined, urodynamic tests typically last about 1 hour and their results are immediate.
-
- These tests are of particular value in making final determinations about bladder function before any surgery is undertaken.
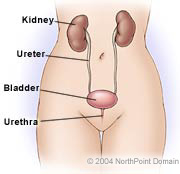
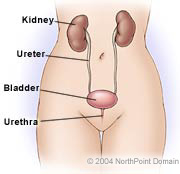
Urodynamics is a series of tests that measure bladder and urethral function performed in patients whose symptoms suggest a problem with the muscles or nerves of the lower urinary system and pelvis. Symptoms that may lead a urologist to order urodynamic testing include:
-
- Difficulty urinating or emptying the bladder;
-
- Involuntarily leakage of urine;
-
- Bladder control problems; or
Urodynamic tests assess problems in the bladder, urethra, and sphincter muscles related to such symptoms by examining the storage of urine in the bladder, the bladder’s pressure response to being filled with fluid or gas (fluid is preferred), and the flow of urine from the bladder through the urethra. Standard urodynamic tests include:
-
- Urethral pressure profile;
-
- Abdominal pressure measurement; and
PRE-TEST GUIDELINES
Patients should not urinate for several hours before the tests.
Patients with active, untreated urinary tract infections (UTIs) should have the infection treated and cleared prior to undergoing the test.
WHAT TO EXPECT
Cystometry. After ensuring that the bladder is empty, a small catheter is inserted and the bladder is filled with a saline solution or carbon dioxide. The catheter is connected to a cystometer, which monitors bladder pressure.
Rarely, drugs may be administered to the patient during cystometry to assess the impact of the medications. A contrast dye can be used to fill the bladder, allowing a physician to take x rays of the bladder and the lower urinary tract.
Electromyography. Electromyography measures the electrical activity of the pelvic muscle. During the cystometry while contractions are occurring, the physician may record the electrical activity of the pelvic muscles. The physician places a needle electrode or patch electrode into or on the pelvic floor muscles, located in the perineum. The electrodes transmit data to a computer screen to show the muscle response to nerve stimulation. Abnormal readings may indicate nerve damage, a hyperactive bladder, or lack of coordination between sphincter relaxation and bladder contractions.
Urethral pressure profile. The urologist may take measurements of the urethral wall as the catheter is removed from the body.
Urinary flow rate. Flowmeters are funnels into which a patient urinates. An attached flowmeter measures and graphically displays urine flow. If a flowmeter isn’t available, medical staff can time urine flow with a stopwatch and then measure the collected urine volume.
POSSIBLE COMPLICATIONS
There are no complications directly associated with urodynamic testing. Catheter insertion may cause slight discomfort following the tests. The discomfort may last for a few hours; drinking two 8-ounce glasses of water every 2 hours may alleviate some of the pain.
Copyright © 2017 NorthPoint Domain, Inc. All rights reserved.
This material cannot be reproduced in digital or printed form without the express consent of NorthPoint Domain, Inc. Unauthorized copying or distribution of NorthPoint Domain’s Content is an infringement of the copyright holder’s rights.